Physical appearance is a common concern associated with the female population, however, a very frequent complain in this context among the males, is gynecomastia. Though a clinically insignificant condition, it can affect any age group and can be a source of embarrassment for the subjects.
Gynecomastia is defined as enlargement of the breast tissue in the male population. It is a benign condition, characterized by a proliferation of the glandular breast tissue secondary to hormonal imbalance, or drugs. Gynecomastia in male population shows three peaks when plotted alongside age; in infancy, puberty and advanced age.
About 60-90% [1] of infants have gynecomastia. In this age, gynecomastia is due to the effect of maternal estrogen. About half of the prepubescent males experience gynecomastia, and with advanced age, its prevalence is about 70%. Due to other abnormalities, gynecomastia may arise at any stage of life, making it a very frequent complaint.
Pathophysiology
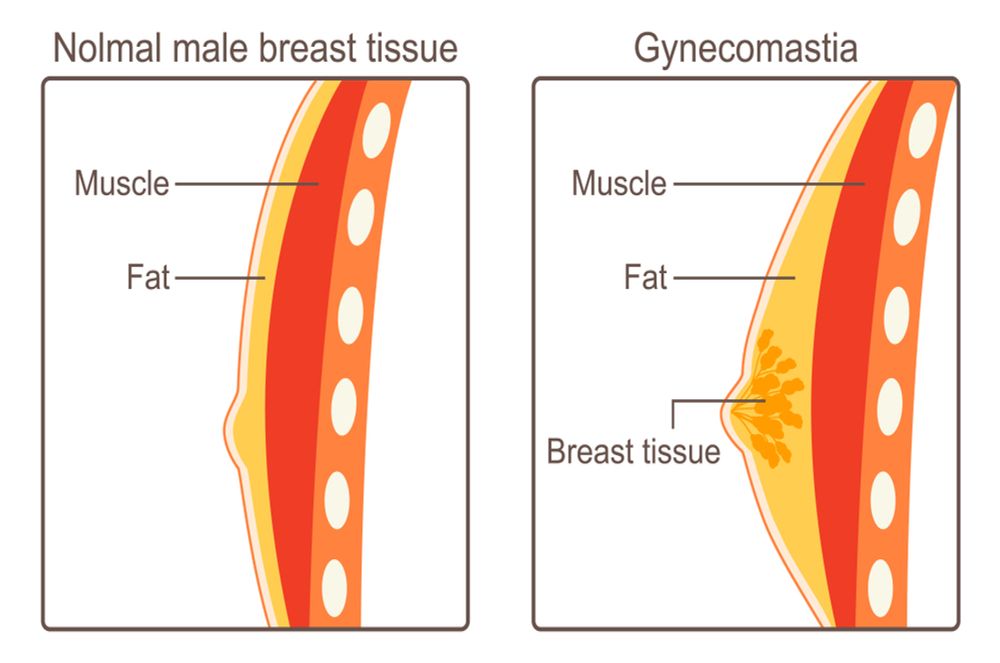
The secondary sexual characteristics are regulated by estrogen levels in females, and androgens in males. Though testosterone is the primary male sex hormone, males do secrete minor amount of estrogen. The balance between these two hormones regulate the breast size in men. An imbalance that leads to increase in estrogen, prompts growth of the glandular component of breast tissue. However, unlike in females, the alveolar component does not proliferate. It also decreases the synthesis and free circulating amount of testosterone, hence, diminishing the contrary effect of testosterone on breast tissue. This imbalance may be due to a congenital condition, side-effect of certain drugs, or age-related physiological changes. This series of events lead to increase in the size of breast in males.
Hence, not only the balance of interconversion of androgens and estrogens, but also the factors which regulate the levels of free circulating amount of these hormones, play a role in manifesting gynecomastia.
Pseudogynecomastia:
Breast enlargement in males as opposed to females, is viewed a stretch from normal physiology. It can be either due to proliferation of the glandular tissue in the pectoral region, or due to deposition of fatty substance in the region. The latter condition that is seen tightly coupled with obesity, is known as pseudogynecomastia. Pseudogynecomastia is reversible, a reduction in weight helps deal with gynecomastia too. The diagnosis of clinical gynecomastia is made after differentiating it from this condition.
Gynecomastia and breast cancer:
The primary concern when faced with gynecomastia is breast cancer. Though, the common risk factor for both, gynecomastia and breast cancer is a high estrogen state, but gynecomastia itself only rarely leads to breast cancer. A study [2] suggests that gynecomastia can increase the chance of breast cancer by 10%. Breast cancer is a rare occurrence in the male population, accounting for 1% of all the breast cancer cases.
In the presentation, breast cancer is usually a unilateral firm mass, whereas, gynecomastia is almost always bilateral diffuse swelling of all of the breast tissue. The family history and evaluation of risk factors in the history of the patient can further help in clarifying the differentials.

