Myasthenia Gravis Pathophysiology
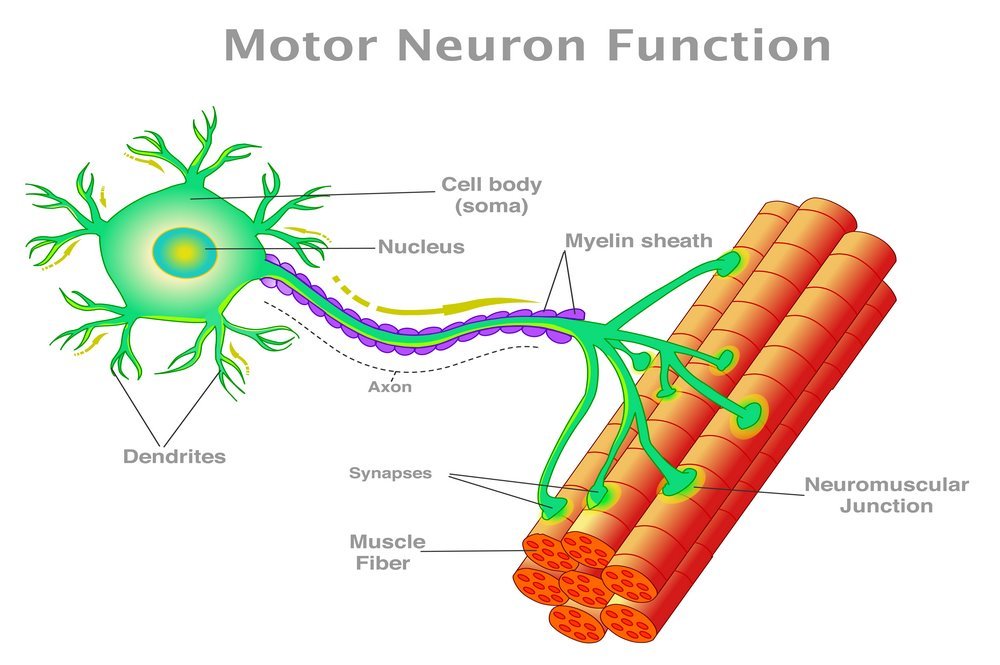
Myasthenia gravis is one of the autoimmune disorders that specifically affects the neuromuscular junction (NMJ) resulting due to the attack of antibodies on the components of postsynaptic membrane. The attack of antibodies disrupts the neuromuscular transmission and leads to fatigue and weakness of the skeletal muscles. There is either localized or generalized weakness which might confine to either a single muscle or group of muscles such as involvement of the respiratory and bulbar muscles that can be life threatening. The studies suggest that the pathophysiological pattern of myasthenia gravis depends on the type and target of the auto-antibodies. In most of the cases, immunoglobulin Ig G1 and Ig G3 antibodies attack the receptors of acetylcholine (AChR). The extent of damage happening to the neuromuscular junction by the auto-antibodies depends on the sensitivity of synapses to acetylcholine receptors and the number of sodium voltage-gated channels. [8]
In addition, the immunoglobulin Ig G1 and Ig G3 antibodies produce damage which is complement-mediated and increase the degree of acetylcholine receptor (AChR) turnover, both of these processes cause more loss of acetylcholine receptors from the postsynaptic membrane. The involvement of thymus gland is present in many patients of myasthenia gravis and the genetic and experimental approaches help in understanding the lack of immune tolerance to acetylcholine receptors. Whereas in the case of patients who test negative for AChR antibodies might need testing for another less common protein, the muscle specific kinase (MuSK). The presence of MuSK antibodies causes impairment of the neuromuscular junction by dissembling the physiological role of MuSK in synapse adaptation and maintenance.
Extensive studies on the synapse function and the autoimmune activity of antibodies gives the idea of how the myasthenia gravis disorder operates. Another study involving the use of microelectrode records the effect of antibodies on the electrical impulse transmission through the neuromuscular junction. A microelectrode helps in recording the electrical potential of the membranes in a certain muscle fiber near the neuromuscular junction. By electrically stimulating the nerve, the neuromuscular transmission of nerves is visible which indicates a short rise in membrane potential known as endplate potential (EPP). The patients of myasthenia gravis indicate a visible decrease in the amplitude of EPP and the vesicle load of AChR, which means that there is lesser electric potential available for the membranes to transfer the nerve impulses.
The progression of myasthenia gravis severely affects the ability of the synapse to allow the smooth and normal transmission of nerve impulses between the muscles and the nerve. There is a smaller EPP which might not reach the required level of the muscle action potential to transmit nerve impulses at the neuromuscular junction. A consecutive failure of the action potential to reach its threshold level leads to the decrement of muscle movements and thus causes weakness or fatigue after periods of activity. Some factors that take part in the variability of muscle weakness among different patients or even within a patient include the higher number of AChR present in the neuromuscular junction to face the attack of antibodies, the mechanisms of synaptic compensation, and the rate of diffusion of AChR antibodies present in each synaptic cleft.
