Pulmonary Embolism Pathophysiology
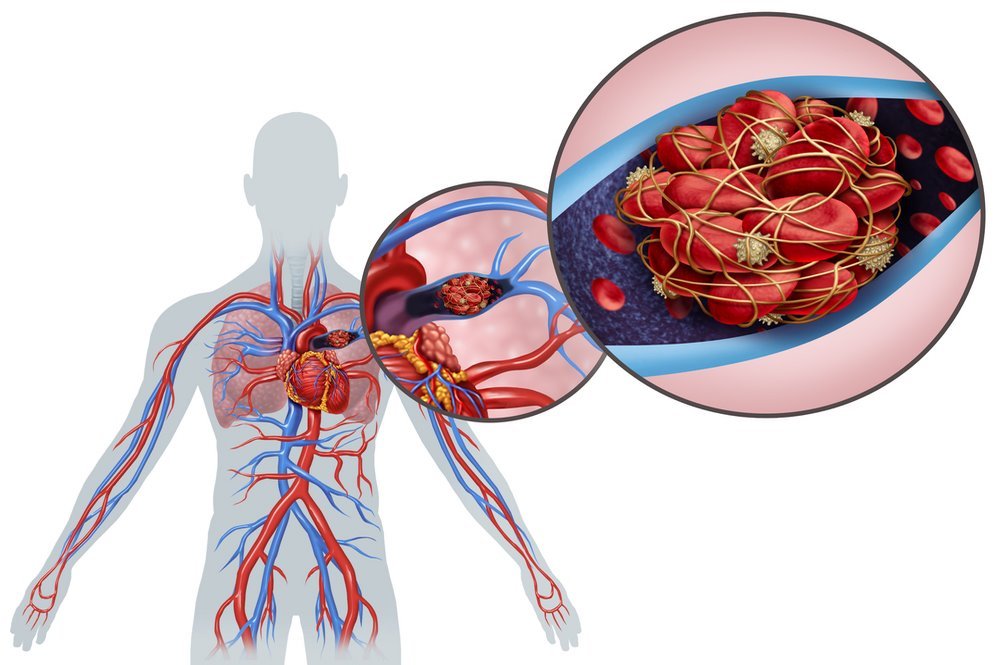
Pulmonary embolism appears when blood clots in deep veins detach and start embolizing in the pulmonary circulation. The blood clots cause vascular occlusion in the lungs and impair blood circulation and gas exchange. The lower lobes in the lungs suffer more frequently than the upper lobes as the involvement of bilateral lung tissues is more common. Larger blood clots starts wedging in the main pulmonary artery while smaller blood clots reside the peripheral arteries. The smaller blood clots living in the peripheral arteries of the lungs lead to the development of intra-alveolar tissue death thus resulting in pulmonary infarction. Pulmonary infarction develops in almost 10% of the pulmonary embolism patients without any underlying cardio-pulmonary condition. [7]
Blockage of the pulmonary arteries creates no area for ventilation as the alveoli need space for ventilation to exceed the blood flow to pulmonary capillaries. The dead space ventilation contributes to the mismatch in ventilation-perfusion rate with vascular obstruction of the arteries and adds up to the pulmonary vascular resistance. Moreover, hormonal mediators such as thromboxanes and serotonin releasing from activated platelets might trigger vasoconstriction in the areas that are not suffering from pulmonary embolism. As the pulmonary artery increases systolic pressure, the after-load on the right ventricle increases which leads to the failure of right ventricle. As the failure of right ventricle progresses, there is development of impairment in left ventricle as well.
Rapid advancement to myocardial ischemia might occur other than the risks of insufficient coronary artery filling, syncope, potential for hypotension, sudden death, or electromechanical dissociation. Abrupt indication of pulmonary embolism is essential because of the high mortality and morbidity rates, which might be a hurdle for early treatment of the condition. as 30% of the pulmonary embolism patients die without getting treatment so there is definitely a failure in diagnosing pulmonary embolism which needs serious management. However, only 8% of the patients survive and live a normal life with an effective treatment course. Unfortunately, pulmonary embolism might be asymptomatic and is present with sudden death.
The characteristic signs and symptoms of pulmonary embolism like Dyspnea, chest pain, shock, tachycardia, and hypoxemia are present and non-specific in many other conditions including congestive heart failure, myocardial infarction, or pneumonia. The prospective studies of pulmonary embolism patient with an early diagnosis report that there is a wide range of symptoms that patients experience and some of them are similar among all. Tachypnea is one of the common signs of pulmonary embolism with a percentage of 54% along with 24% tachycardia. The next common symptoms was dyspnea, usually begins within seconds of the onset of the disease, with exertion or at rest dyspnea was 73%, calf or thigh pain was common among 44% of the patients and plueritic pain was common among 44% of the patients. In addition, there was 34% cough symptom and 41% calf or thigh swelling symptom among pulmonary embolism patients. Only 24% of the patients represent tachycardia as the most commonly occurring symptoms in comparison to the other signs and symptoms. However, the critically ill patients with kidney failure or with higher creatinine levels are not part of these studies, because the pulmonary embolism takes different ways to develop in these cases.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3665123/
